Ovarian cancer is a terrible disease, almost impossible to find early before it has spread and very hard to cure despite the best efforts over the past 40 years. As a result, it had been common practice to remove ovaries when a hysterectomy was performed in order to prevent the future development of ovarian cancer. However, it has also been known for 40 years that the ovaries continue to produce hormones after menopause (and forever), although in smaller amounts. I have been the principal author of three studies that show that women who have their ovaries removed had a higher risk of death from heart attack, lung cancer and colon cancer (abstracts below). As a result, I have been encouraging women to keep their ovaries if they had to have a hysterectomy, unless they were at known high-risk of ovarian cancer due to the BRCA genes or a strong family history.
Surprisingly, in the past few years, it has become clear that the most aggressive types of “ovarian” cancer don’t start in the ovaries at all. Most “ovarian cancer” actually starts in the fallopian tube and some of these cancers start in the uterine lining cells that are shed and pass out the ends of the tubes during a normal menstrual period. So, after all of these years, most “ovarian” cancer is, in fact, fallopian tube or uterine lining cell cancer. Since the fallopian tubes are open at the end, this explains why the cancer spreads so quickly and easily. It also explains why screening for early ovarian cancer by looking at the ovaries with ultrasound has been such a dismal failure.
After this recent discovery of “fallopian tube cancer”, a number of hospitals in Canada and Europe began recommending that women have their fallopian tubes removed, rather than their ovaries, when they were having hysterectomies. I have been concerned though, since the tube and ovary share some common blood vessels, that removal of the tube might reduce blood flow to the ovaries and diminish hormone production. If this were the case, women still might end up with the long-term health consequences that we found in the studies we did (abstracts below).
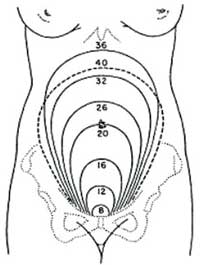
The good news is that a new study, just published in Gynecologic Oncology, shows that ovarian function as measured by a number of blood and ultrasound tests (AMH, FSH, ovarian volume and antral follicle counts) remains normal following removal of the tubes. As a result, it appears to be safe to remove the tubes. I am, therefore, going to start discussing with all of my patients who do not want any more children, the option of removing the fallopian tubes at the time of pelvic surgery for any reason: myomectomy, ovarian cyst removal, hysterectomy, etc.
My thought, which I am going to write in a letter to the editor of Gynecologic Oncology, is that gynecologists should also start teaching general surgeons how to perform removal of the tubes and that any woman (not interested in childbearing) who is having abdominal surgery should consider removal of the fallopian tubes at the same time.
Ovarian cancer has been a frustrating story, but now it likely has a happy ending – hopefully, the prevention of most tubal (“ovarian”) cancers that have caused so much ill health, death and fear.
Our research, showing the benefit of keeping your ovaries, will end up as part of the larger story; since ovarian cancer was never ovarian, the ovaries should never have been removed all along!
References
Prophylactic Salpingectomy in Premenopausal Low-risk Women for Ovarian Cancer: Primum non nocere.
Morelli M, Venturella R, Mocciaro R, Di Cello A, Rania E, Lico D, D’Alessandro P, Zullo F. Gynecologic Oncology. 2013;129:448-51.
Long-Term Mortality Associated With Oophorectomy Compared With Ovarian Conservation in the Nurses’ Health Study.
Parker WH, Feskanich D, Broder MS, Chang E, Shoupe D, Farquhar CM, Berek JS, Manson JE.
Obstetrics and Gynecology. 2013;121:709-716.
OBJECTIVE: To report long-term mortality after oophorectomy or ovarian conservation at the time of hysterectomy in subgroups of women based on age at the time of surgery, use of estrogen therapy, presence of risk factors for coronary heart disease, and length of follow-up.
METHODS: This was a prospective cohort study of 30,117 Nurses’ Health Study participants undergoing hysterectomy for benign disease. Multivariable adjusted hazard ratios for death from coronary heart disease, stroke, breast cancer, epithelial ovarian cancer, lung cancer, colorectal cancer, total cancer, and all causes were determined comparing bilateral oophorectomy (n=16,914) with ovarian conservation (n=13,203).
RESULTS: Over 28 years of follow-up, 16.8% of women with hysterectomy and bilateral oophorectomy died from all causes compared with 13.3% of women who had ovarian conservation (hazard ratio 1.13, 95% confidence interval 1.06-1.21). Oophorectomy was associated with a lower risk of death from ovarian cancer (four women with oophorectomy compared with 44 women with ovarian conservation) and, before age 47.5 years, a lower risk of death from breast cancer. However, at no age was oophorectomy associated with a lower risk of other cause-specific or all-cause mortality. For women younger than 50 years at the time of hysterectomy, bilateral oophorectomy was associated with significantly increased mortality in women who had never used estrogen therapy but not in past and current users: assuming a 35-year lifespan after oophorectomy: number needed to harm for all-cause death=8, coronary heart disease death=33, and lung cancer death=50.
CONCLUSIONS: Bilateral oophorectomy is associated with increased mortality in women aged younger than 50 years who never used estrogen therapy and at no age is oophorectomy associated with increased survival.
LEVEL OF EVIDENCE: I
Ovarian Conservation at the Time of Hysterectomy and Long-term Health Outcomes in the Nurses’ Health Study.
Parker WH, Broder MS, Chang E, Feskanich D, Farquhar C, Liu Z, Shoupe D, Berek JS, Hankinson S, Manson JE.
Obstetrics and Gynecology. 2009;113:1027-37.
OBJECTIVE: To report long-term health outcomes and mortality after oophorectomy or ovarian conservation.
METHODS: We conducted a prospective, observational study of 29,380 women participants of the Nurses’ Health Study who had a hysterectomy for benign disease; 16,345 (55.6%) had hysterectomy with bilateral oophorectomy, and 13,035 (44.4%) had hysterectomy with ovarian conservation. We evaluated incident events or death due to coronary heart disease (CHD), stroke, breast cancer, ovarian cancer, lung cancer, colorectal cancer, total cancers, hip fracture, pulmonary embolus, and death from all causes.
RESULTS: Over 24 years of follow-up, for women with hysterectomy and bilateral oophorectomy compared with ovarian conservation, the multivariable hazard ratios (HRs) were 1.12 (95% confidence interval [CI] 1.03-1.21) for total mortality, 1.17 (95% CI 1.02-1.35) for fatal plus nonfatal CHD, and 1.14 (95% CI 0.98-1.33) for stroke. Although the risks of breast (HR 0.75, 95% CI 0.68-0.84), ovarian (HR 0.04, 95% CI 0.01-0.09, number needed to treat=220), and total cancers (HR 0.90, 95% CI 0.84-0.96) decreased after oophorectomy, lung cancer incidence (HR=1.26, 95% CI 1.02-1.56, number needed to harm=190), and total cancer mortality (HR=1.17, 95% CI 1.04-1.32) increased. For those never having used estrogen therapy, bilateral oophorectomy before age 50 years was associated with an increased risk of all-cause mortality, CHD, and stroke. With an approximate 35-year life span after surgery, one additional death would be expected for every nine oophorectomies performed.
CONCLUSION: Compared with ovarian conservation, bilateral oophorectomy at the time of hysterectomy for benign disease is associated with a decreased risk of breast and ovarian cancer but an increased risk of all-cause mortality, fatal and nonfatal coronary heart disease, and lung cancer. In no analysis or age group was oophorectomy associated with increased survival.